| REGULATION OF TOTAL BODY FAT STORES
|
| Adipose tissue is an active endocrine organ
|
| page 204 |  | | page 205 |
| Figure 15.5 Elongation of fatty acids. Fatty acid elongation occurs on the endoplasmic reticulum and is carried out by another enzyme complex, fatty acid elongase. |
| It has been long understood that increased energy intake without appropriate increase in energy expenditure is
associated with increased adiposity, in terms both of the numbers of adipocytes and of their fat content - that is, obesity. It is now clear that the adipose tissue is hormonally active. Hormone-like substances such as leptin, adiponectin, and resistin (collectively termed adipokines), growth factors such as vascular endothelial growth factor (VEGF), and pro-inflammatory cytokines (tumor necrosis factor alpha (TNF-α) and interleukin 6 (IL-6)) are all generated by the adipocytes. The main molecules which carry information related to the size of the fat stores (adiposity signals) are leptin, generated in the adipose tissue, and insulin, synthesized in the pancreas. The amount of leptin present in blood is proportional to the body fat content. Leptin regulates food intake and energy expenditure, and also has neuroendocrine function. It decreases appetite and increases thermogenesis. Animals deficient in leptin are hyperphagic and obese. Inefficient leptin action decreases fat oxidation, increases tissue TAG content and increases insulin resistance (Chapter 20). On the other hand, in normal animals, leptin treatment causes hypophagia, leads to increased oxidation of the fatty acid, depletion of tissue TAG, and to an increase in insulin sensitivity. Leptin crosses the blood-brain barrier.
|
Another adipokine, adiponectin, is specific to the adipose tissue. It has an insulin-sensitizing effect: it decreases glucose and non-esterified fatty acid concentrations in plasma without affecting insulin concentration. (See also Chapter 21.) and non-esterified fatty acid concentrations in plasma without affecting insulin concentration. (See also Chapter 21.)
|
| Insulin also plays a role in regulating food intake: it decreases appetite; deletion of insulin receptor in experimental animals leads to hyperphagia. Interestingly, both insulin and leptin signalling pathway involves phosphatidyl inositol-3-kinase (PI-3 kinase). This is an example of a pleiotropic (multifunctional) role of key signal transduction molecules. Leptin also signals through the JAK-STAT system (see Chapter 38).
|
| Figure 15.6 Desaturation of fatty acids. Human desaturases cannot introduce a double bond between carbon 9 and the methyl (ω) end of the fatty acid. This (CH2)7 represents the limit at which a double bond can be introduced. cyt b5, cytochrome b5; FAD, flavin adenine dinucleotide; FADH2, reduced flavin adenine dinucleotide; Fe3+, ferric ion. |
| page 205 |  | | page 206 |
| Figure 15.7 Triacylglycerol synthesis. Triacylglycerols (TAGs), also called triglycerides, are synthesized in adipose tissue and the liver. The source of glycerol-3-P is different in the two tissues, because there is no glycerol kinase in adipose tissue. |
| A 48-year-old ex-Army infantryman (height 1.91 m) presented with the problem of increasing weight over the previous 8 years since leaving the Army. At the time of his retirement from active service, he had weighed 95 kg (209 lb) but at presentation weighed 193 kg (424.6 lb). His current occupation was that of truck driver. He denied any change in food intake since leaving the Army, but admitted to taking little or no exercise. Detailed enquiry indicated that his daily dietary intake provided between 12 600 and 16 800 kJ (3000 and 4000 kcal), with a fat intake approaching 40%. The patient was initially placed on a healthy eating plan, with fat intake reduced to 35% of total calories. He was advised to exercise and proceeded to swim three or four times per week. His weight immediately began to decrease, rapidly at first, and then at 3-4 kg (6.6-8.8 lb) each month until it stabilized at 145-150 kg (319-330 lb). He was then placed on a high-protein/low-carbohydrate/low-fat diet, which induced a return of weight loss that continued for a further year, resulting in a final weight of 93 kg (204.6 lb). |
Comment. Obesity is increasingly prevalent in many parts of the world. Clinical obesity is now clearly defined in terms of height and weight through the body mass index (BMI), which is calculated as the weight in kilograms divided by the (height in meters)2 (see Chapter 12 for details):
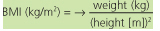 |
| BMI 25-30 kg/m2 is classified as overweight or grade I obesity, BMI >30 kg/m2 is clinical or grade II obesity, and BMI >40 kg/m2 is classified as morbid or grade III obesity. Our patient had a BMI of 53 at presentation falling to 26 after prolonged diet. If energy input exceeds output over time then weight will increase. Obesity predisposes to several diseases. The most important is type 2 diabetes mellitus: 80% of this type of diabetes is associated with the obese state. Other associated illnesses include coronary heart disease, hypertension, stroke, arthritis, and gall bladder disease. (See also Chapter 21.) |
| page 206 |  | | page 207 |
| Figure 15.8 Transport and storage of fat in response to feeding. The relationship between the biosynthesis of fatty acids in the liver, their export as VLDL, and increased storage of fat as triacylglycerols (TAGs). Insulin is an important regulator of this pathway. In the liver, it stimulates glycolysis, thereby increasing pyruvate production. It activates the pyruvate dehydrogenase complex (by causing its dephosphorylation), and thus promotes synthesis of acetyl-CoA. This stimulates the TCA cycle and increases the concentration of citrate. Citrate stimulates acetyl-CoA carboxylase, increasing the rate of fatty acid biosynthesis. F-1,6-BP, fructose-1,6 biphosphate; IDL, intermediate-density lipoprotein. (See also Chapter 17 for details of lipoprotein metabolism.) |
|