| Bone serves as a store of calcium
|
| A complex calcium homeostatic mechanism utilizes bone as the reservoir of calcium when deficiency exists, and as a store of calcium when the body is replete.
|
| The skeleton contains 99% of calcium present in the body in the form of hydroxyapatite; the remainder is distributed in the soft tissues, teeth, and ECF. Many cell and organ functions are dependent on the tight control of extracellular calcium concentration; these include neural transmission, cellular secretion, contraction of muscle cells, cell proliferation, the stability and permeability of cell membranes, blood clotting, and the mineralization of bone. Total serum calcium is maintained between 2.2 and 2.60 mmol/L (8.8-10.4 mg/dL).
|
| Hormonal control of circulating calcium involves bone, kidneys, and the gastrointestinal tract
|
| Hormonal control of circulating calcium involves bone, kidneys, and the gastrointestinal tract: if plasma calcium decreases, PTH is released from the parathyroid glands, stimulating osteoclast-mediated bone resorption, reabsorption of calcium at the kidney, and absorption of calcium at the small intestine (mediated by 1,25(OH)2D3); increasing calcium decreases PTH secretion and stimulation of calcitonin release from the thyroid, which inhibits osteoclast resorption of bone (Fig. 24.2).
|
Calcium exists in the circulation in three forms (Fig. 24.3):
- ionized Ca2+: the most important, physiologically active form (50% of total calcium).
- protein-bound: the majority of the remaining calcium, mainly bound to negatively charged albumin (40%);
- complexed to substances such as citrate and phosphate: a smaller fraction (10%).
|
| Figure 24.2 Major hormones influencing calcium homeostasis. A decrease in plasma ionized calcium stimulates release of PTH; this promotes Ca2+ reabsorption from the kidney, resorption from bone, and absorption by the gut via increased production of 1,25(OH)2D3. As a result, plasma calcium increases. Conversely, an increase in plasma ionized calcium stimulates release of calcitonin, which inhibits reabsorption of calcium by the kidney and osteoclast-mediated bone resorption. |
| page 347 |  | | page 348 |
| Figure 24.3 Circulating calcium fractions. The three forms of circulating calcium. |
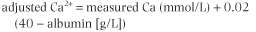
If serum protein concentration increases (as in dehydration and after prolonged venous stasis), protein-bound calcium and total serum calcium increase. In conditions of reduced serum proteins (e.g. liver disease, nephrotic syndrome, malnutrition), the protein-bound calcium concentration is reduced, decreasing the total calcium, although ionized calcium is maintained within the reference range 1.1-1.3 mmol/L (4.4-5.2 mg/dL). Many acute and chronic illnesses decrease serum albumin concentration, which consequently decreases serum total calcium. Because of this, in clinical situations it is important to calculate the 'adjusted calcium' - total serum calcium, adjusted for the patient's prevailing albumin concentration. This is achieved by means of a formula utilizing the population mean albumin concentration 40 g/L (4 g/dL):
|
|